You can find a million articles, research studies, and blog posts about the benefits of breastfeeding. Is there really a difference between breastfeeding and feeding a baby formula? That subject, ” Risks of NOT Breastfeeding”, can trigger some serious emotional responses in many people. Some people choose not to breastfeed and some have no control over certain situations, or feel that choosing formula is their best or only choice for the situation. In this post we will be dealing with the risks to your baby of not breastfeeding. But I want to emphasize that the purpose of this post is to inform and to educate and not to make someone feel bad or “less than”, especially for a decision that may have been totally out of their control. The best decisions are made when we have all of the information, alternatives, benefits, and risks. Remember, the BRAIN acronym can be applied to lots of situations.
B.R.A.I.N.
BENEFITS, RISKS, ALTERNATIVES, (use your) INTUITION, (do) NOTHING
See Related Content: Bring Your Brain to Your Birth
RISKS OF NOT BREASTFEEDING FOR BABIES
In addition to these statistics from the U.S. Department of Health and Human Resources, below, do your own research and reading. Some recommended reading containing facts and science are (affiliate links):
There are many research studies that show that full-term infants who are fed artificial baby milk/formula have greater risks* of:
- Childhood obesity – 32% increased risk
- Type 1 and type 2 diabetes – 64% increased risk
- Leukemia – 18-23% increased risk
- SIDS (Sudden Infant Death Syndrome) – 56% increased risk
- Asthma with no family history – 35% increased risks
- Asthma with family history – 67% increased risk
- Acute ear infection – 100% increased risk
- Hospitalization for lower respiratory tract diseases in the first year 257% increased risk
- Eczema – 47% increased risk
*Source U.S. Department of Health and Human Services, Office of the Surgeon General 2011
Artificial Baby Milk VS Breast Milk
It is generally accepted that feeding babies formula/artificial baby milk is good or even normal. Back in the day when I was an infant, doctors were telling mothers that formula was better or as good as breastmilk. For many people, this is “just what you feed a baby”. It’s normal, accepted, expected. There is a perception that breastfeeding is just a little extra bonus or “frosting on the cake” or like giving your baby extra vitamins. What most people don’t know is that choosing formula presents possible long-term negative effects on the infant’s health and development, and also the health of the mother.
3 Types of Formula
- Cow’s milk based – This is the base for the majority of artificial baby milk brands.
- Soy based – Plant protein is the base and may be good for babies who cannot tolerate lactose, or are allergic to cow’s milk.
- Hydrolisate protein –Proteins are broken down so that the formula is easier for baby to digest. These formulas tend to be much more expensive. But may be the only option if a child is allergic to cow’s milk or soy.
Formula is similar to breastmilk because it provides nourishment, energy, and hydration. Sometimes it ends up being our only choice. Certain health conditions, circumstances around the birth, or not getting education or support for breastfeeding can lead to the need to use artificial baby milk. As I have learned from my friend and lactation consultant, Kimberly Murphy, ICBLC, your #1 Job is to “Feed the Baby”. She even has a bracelet that has that engraved on it. As moms, we can only do our best, and sometimes that means turning to alternatives to our own breastmilk. We know from study after study that breastmilk is best and I don’t want to vilify the moms who choose formula or feel they have no other choice. My goal is to present the facts as best I can, so a new mother can decide what is best for her and her baby.
What’s in Formula?
Of course, the ingredients in baby formula will differ from brand to brand. In general, you’ll find:
- Lactose or other sugars like corn syrup, fructose
- Oils such as palm oil, coconut oil, sunflower oil, soybean oil
- Fatty acids derived from fish oils
- Vitamins and minerals
- Some have pre-biotics and probiotics
- Some have DHA
- Amino acids
- Enzymes
As an example, let’s take the ingredients in the ingredient list on a can of Similac.
Here are the first four ingredients in a can of Similac, a soy based formula:
- 42.6% corn syrup solids,
- 14.7% Soy Protein Isolate (which means the proteins have been broken down so that baby will be able to digest it),
- 11.5%high oleic safflower oil,
- 10.1% sugar(sucrose).
When you look at the individual ingredient list, it can seem a bit scary. These infant formulas are highly processed foods so that babies can digest them, and they contain a lot of things. The list goes on and on. Millions of dollars have gone in to the research to find the best food for your baby. But look at just the soy protein. A baby drinking soy-based formula is getting an extraordinary amount of estrogen-like compounds. One study published in the Journal of Clinical Endocrinology and Metabolism, 2018 found “Infants who consumed soy-based formula as newborns had differences in some reproductive-system cells and tissues, compared to those who used cow-milk formula or were breastfed, according to a new study.” Studies have not been done to see if there are long-term effects from the use of artificial baby milk.
It Doesn’t Have to Be All Formula or All Breastmilk
Sometimes, circumstances make it impossible to exclusively feed the baby the mother’s own breastmilk. There are options to exclusively feeding your baby your own breastmilk. Options:
- Pump as much of your own milk to give to your baby, even if it’s 1-2 oz/day. It doesn’t have to be all formula or all breastmilk. Even a small amount of your own breastmilk or someone else’s is better than none.
- There are organizations that bank human milk, so that all infants have access to breastmilk. You can contact the Human Milk Banking Association. You can also search for “Mother’s Milk Banks near me”. All breastmilk is screened, tested, and pasteurized to get rid of any harmful bacteria or organisms.
- Locally, San Diego Mothers’ Milk Bank at UCSD opened in 2019. There’s even an app in the app store called MothersMilk
- Find a milk bank
- WIC program. Breastfeeding mothers supported by WIC may receive peer counselor support, an enhanced food package, breast pumps, and other supplies. Breastfeeding mothers can also participate in WIC longer than non-breastfeeding mothers. Many WIC offices have an IBCLC as well.
- OWH Helpline (800-994-9662). The Office on Women’s Health Helpline is staffed with breastfeeding peer counselors who can answer your breastfeeding questions in English or Spanish, support you through breastfeeding challenges, and connect you with other resources to help if needed.
Why Choose Breastmilk – Even Someone Else’s Breastmilk?
Breastmilk isn’t just food:
- It is an immune system boost, full of antibodies and white-blood cells.
- It has hormones that foster bonding, regulate appetite, and sleep/wake patterns.
- It is loaded with pre-biotics and probiotics and good bacteria to protect the digestive system.
- The fatty acids in breastmilk help your baby’s brain, nervous system, and eyes develop.
- Your breastmilk has enzymes to help your baby digest the milk.
- Breastmilk contains over 60% whey protein and 40% casein. There are proteins that inhibit organisms, like yeast, protect the infant from viruses, and bad bacteria, and it contains good bacteria that protects the baby from harmful bacteria.
- There are essential fat-soluble vitamins in breastmilk, like A,D,E,K.
- Lactose is the primary carbohydrate and helps promote healthy bacteria growth.
Be Absolutely Sure You CAN’T Breastfeed
So many women think that they can’t breastfeed for a variety of reasons. To be absolutely sure, see a lactation consultant, not just your pediatrician. Many pediatricians know very little about breastfeeding. I know that’s a shocking statement. But, sadly, it is a true statement. See a lactation consultant a minimum of three times to be sure there is a medical reason you cannot breastfeed. You can find a lactation consultant here. You can also find breastfeeding support groups through U.S. Breastfeeding.org or through La Leche League International.
The First 10-14 Days Are Essential in Establishing Milk Supply
Right after your body expels the placenta, you have high levels of prolactin, the milk hormone, that has been supplied by your placenta. But postpartum, daily, those prolactin levels decrease. So you literally have the first 10-14 days to tell your body you need milk for your baby. And to let your pituitary gland know you need to make milk.
If you are able to breastfeed, make sure you are feeding your baby a minimum of 8 times in 24 hours. You can feed your baby 8-12, or more, times if you’re able. These first two weeks is a significant time to put in your “food order” to let your body know that you’re going to need to make milk for your baby. The more often you do it, the more your body will respond. Every time you remove milk from the breast you are signaling to your brain, “Make More Milk!”
If you are not able to breastfeed because your baby is in the NICU, or your milk volume increase is delayed because of birth complications or medications or illness, you can still signal your body to make milk. You will need to get help from the nurses and lactation consultants at the hospital to find the right breast pump for your needs. Pump a minimum of 8 times and possibly up to (or even more than) 12 times in 24 hours. Set your alarm and don’t skip a single pumping session and pump both breasts 10-15 minutes per pumping session. You have a small window of time to get a good start – 10-14 days postpartum.
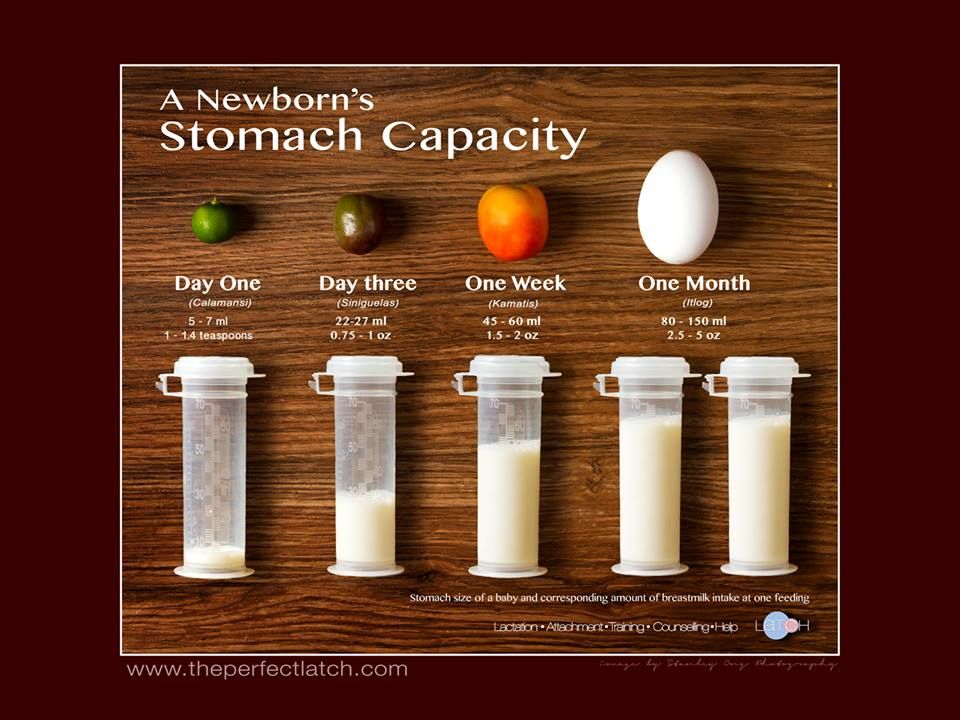
Don’t make breaks between pumping sessions grow longer. It is so important. Many moms see so little milk, that they may give up. Refer to the photo above and you can see how little milk your baby actually needs per feeding. But the more often you remove milk from the breast, the greater your chance of successfully continuing to breastfeed, and continue to make enough milk to feed your baby. Keep a record of how much milk you are getting per pumping session and how often you are pumping. If the volume decreases, contact your lactation consultant ASAP.
Remember that you can only do your best, give it your best shot, and accept that…
“There is no such thing as a perfect mother, but there are a million ways to be a good one” Jill Churchill
Sources:
- The Risks of Not Breastfeeding for Mothers and Infants National Institute of Health
- Women’sHealth.gov – Making the Decision to Breastfeed